Mental Health for Doctors: Tackling Burnout Amidst the NSW Psychiatrist Shortage
Posted 29th Jan 25
Updated 8 months ago
What Does It Take to Become a Psychiatrist in Australia? 🧠📚
Becoming a psychiatrist requires over a decade of training, reflecting the complexity of mental health care. The pathway includes:
-
Medical School (4–6 years) – A foundation in general medicine.
-
Internship (1 year, PGY1) – Hands-on hospital experience across medical specialties.
-
Residency (1+ years, PGY2+) – Additional hospital training before specialisation.
-
Unaccredited Registrar (1+ years, PGY3-5) — Shopping around to make sure it’s for you
-
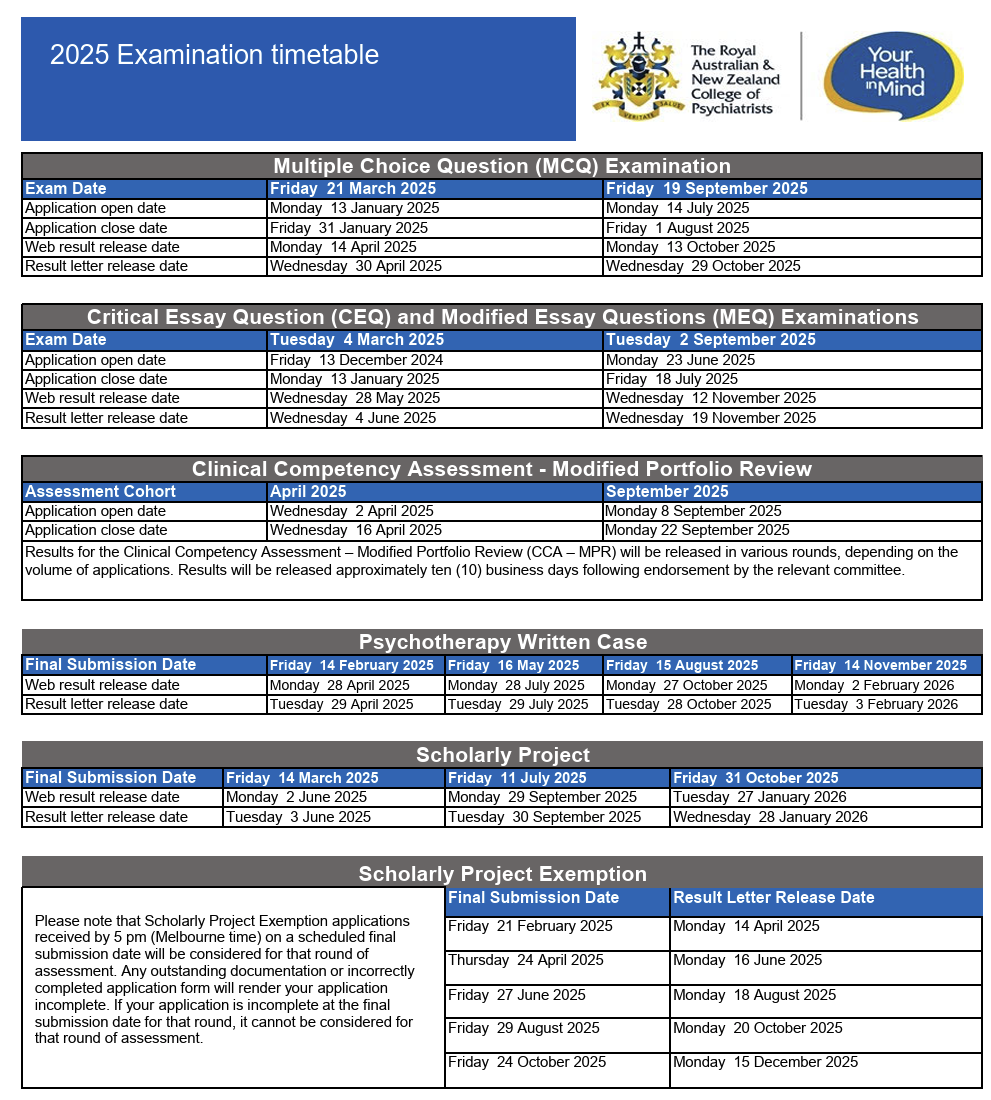
Psychiatry Training (5+ years, PGY4-12) – Supervised work in various psychiatric specialties under the Royal Australian and New Zealand College of Psychiatrists (RANZCP), with multiple exams as seen below.
Despite the long and demanding training required, psychiatrists enter the field to help Australians in need. Psychiatry is a career of compassion, where professionals dedicate themselves to improving mental health, supporting vulnerable patients, and making a real difference in people’s lives. Their work is crucial in addressing the rising mental health challenges faced by Australians today.
It’s not all campfires and marshmallows as we can see…
What Is Causing the Psychiatrist Crisis in NSW? 🚨
The NSW mental health system is in crisis due to chronic workforce shortages and wage disparities.
- 29% of public hospital psychiatry positions are vacant, increasing pressure on remaining doctors.
- NSW psychiatrists earn nearly 30% less than those in Victoria and Queensland, making recruitment difficult.
- Over 200 public psychiatrists have resigned, demanding a 25% pay increase to address pay parity and improve retention.
These resignations, effective from January 21, 2025, could destabilise the public mental health system, leaving patients without critical care with the ripple effects already showing. (Source)
How Will This Shortage Affect Mental Health Services? 🏥🆘
The psychiatrist exodus has serious consequences for both patients and healthcare workers.
- Longer wait times – Patients needing psychiatric care could wait months for appointments.
- Overcrowded emergency departments – With fewer psychiatrists available, patients may turn to hospitals, increasing pressure on emergency staff.
- Increased doctor burnout – The remaining psychiatrists are at risk of exhaustion, making retention even harder.
Without urgent action, mental health care access in NSW will continue to decline. (Source)
How Is Medlo Supporting Doctors’ Mental Health? ❤️🩹
Psychiatrists dedicate their careers to caring for others, yet many are struggling with burnout and exhaustion. RANZCP’s 2024 Workforce Report highlighted the severity of the issue:
- 7 in 10 psychiatrists (73%) report experiencing symptoms of burnout in the past three years.
- 79% of psychiatrists report feeling exhausted and drained all the time.
- 80% report reduced work satisfaction and a loss of motivation to work.
- Almost 33% of psychiatrists are considering leaving the profession within the next three years.
- 9 in 10 trainees (90%) experience burnout—the highest rate among different career stages.
The primary drivers of burnout include workforce shortages (82%), under-resourcing (80%), and excessive workloads (72%). These factors not only impact doctors’ well-being but also compromise patient care, with more than 90% of psychiatrists stating that workforce shortages negatively affect their ability to provide care.
At Medlo, we recognise the urgent need to prioritise mental health support for doctors. That’s why we’ve partnered with Wombat Health to offer practical solutions:
✅ Free access to Wombat Health’s burnout app for doctors who sign up—no shift bookings required.
✅ 10% discount on the first therapy session for Medlo-affiliated doctors.
✅ A focus on preventative care – Helping doctors recognise burnout early and providing tools to manage stress.
The NSW psychiatrist crisis has put a spotlight on doctor burnout, making it clear that systemic change is needed to ensure psychiatrists are supported in their roles. Without urgent action, our ability to continue delivering essential mental health care to patients across Australia is at risk. Supporting doctors' well-being isn’t just about workforce retention—it’s about safeguarding the future of mental health care in this country.
The Project delivered an excellent coverage of the NSW crisis in an interview with Dr. Pramudie Gunaratne (MD, BMed, BA, MMed (Psychiatry), MSc (Public Health), FRANZCP, GAICD). Dr. Gunaratne, Co-Founder and Director of Seriph Clinics, leads a specialist psychiatry practice dedicated to addressing the mental health needs of individuals with complex neuropsychiatric and general psychiatric conditions.
Watch the full interview here: YouTube Link.
What Needs to Happen to Fix This Crisis? 🔄
To prevent further deterioration of NSW’s mental health services, key changes must happen:
🏛️ Government action – Addressing pay disparities and improving working conditions to attract and retain psychiatrists.
⚕️ Support for doctors’ mental health – Providing access to mental health services to reduce burnout.
👥 Better public funding – Advocating for increased investment in mental health services.
At Medlo, we are committed to supporting mental health professionals by offering better work options and mental health resources.
Final Thoughts
The NSW psychiatrist shortage highlights serious flaws in the public mental health system. Without action, patients and doctors will continue to suffer.
While broader reforms are needed, Medlo is stepping up to provide immediate mental health support for doctors. If you’re a psychiatrist looking for support, join Medlo today. 💙